by Russell Noga | Updated May 14th, 2025
In 2026, Medicare will see significant changes to Medicare in 2026 affecting payments, prescription drug coverage, and out-of-pocket costs. These updates will directly impact beneficiaries’ choices and expenses. This article covers the key changes you need to know to stay informed and prepared.
Key Takeaways
- Medicare Advantage plans will see a 5.06% payment increase in 2026, along with a new risk adjustment model to improve payment accuracy and efficiency.
- Medicare Part D will introduce caps on out-of-pocket drug costs and insulin co-pays, along with zero cost-sharing for adult vaccines, improving affordability for beneficiaries.
- Annual review of Medicare plans is crucial for beneficiaries to adapt to changes in healthcare needs, costs, and benefits, ensuring optimal coverage.
Compare 2026 Plans & Rates
Enter Zip Code
Medicare Advantage Plan Payment Updates
One of the most notable changes coming in 2026 is the increase in payments to Medicare Advantage plans. The Centers for Medicare & Medicaid Services (CMS) has finalized a 5.06% increase in payments for Medicare Advantage plans, reflecting the growing costs and needs of Medicare beneficiaries. This increase is part of a broader effort to ensure that Medicare Advantage and part plans remain a viable option for enrollees by providing adequate funding to cover their healthcare needs.
Additionally, the effective growth rate for Medicare Advantage plan payments in 2026 is set at 9.04%, a significant jump that underscores the program’s commitment to adapting to changing healthcare costs. This growth rate is crucial for maintaining the sustainability of Medicare Advantage plans and ensuring that they can continue to offer comprehensive coverage to beneficiaries, including MA payments.
Finally, CMS expects a coding trend to increase average risk scores by approximately 2.10% due to enhancements in the risk adjustment model and risk score calculations. This adjustment aims to more accurately reflect the health status of enrollees, ensuring that payments to Medicare Advantage plans are better aligned with the actual costs of care. These updates highlight the dynamic nature of the Medicare program and the ongoing efforts to improve its efficiency and effectiveness.
New Risk Adjustment Model for Medicare Advantage
The introduction of the new risk adjustment model for Medicare Advantage plans is another significant update for CY 2026. The implementation of the 2024 CMS-HCC risk adjustment model will be fully realized in 2026, which will affect how risk scores are calculated for enrollees. This model aims to enhance payment accuracy and reduce administrative burdens, ultimately leading to a more efficient system for both providers and beneficiaries.
A noteworthy change is the finalized blended risk score for PACE (Program of All-Inclusive Care for the Elderly) organizations and ma organization. This blended score will combine elements from both the 2024 and 2017 CMS-HCC models, providing a more comprehensive and accurate assessment of enrollees’ health status. This change is expected to streamline the process and improve the accuracy of payments to PACE organizations.
Additionally, CMS proposed implementing a three-year phase-in for adjustments related to medical education costs for MA enrollees of Medicare Advantage enrollees, with advance notice provided to ensure a smoother transition and help ensure that the adjustments are integrated effectively without causing disruptions in care.
These updates to the risk adjustment model are part of a broader effort to refine the Medicare Advantage program and enhance its overall performance.
Changes to Medicare Part D Prescription Drug Coverage
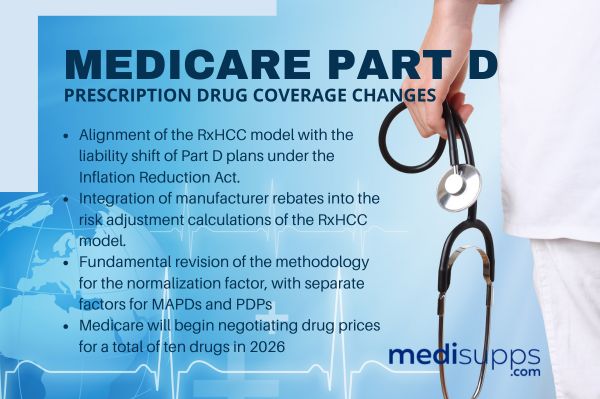
Significant changes are also coming to Medicare Part D prescription drug coverage in 2026. One of the key updates is the alignment of the RxHCC model with the liability shift of Part D plans under the Inflation Reduction Act. This alignment is designed to ensure that the model accurately reflects the costs and risks associated with prescription drug coverage.
Another important change is the integration of manufacturer rebates into the risk adjustment calculations of the RxHCC model. This integration aims to provide a more accurate representation of the net costs of prescription drugs, which will help in setting fair and reasonable prices for beneficiaries.
The 2026 changes also include a fundamental revision of the methodology for the normalization factor, with separate factors for MAPDs (Medicare Advantage Prescription Drug plans) and PDPs (Prescription Drug Plans). This separation will allow for more precise adjustments based on the specific characteristics of each plan type, including ma plans. Normalization factors for 2026 are as follows, in accordance with the Part D final rule. The factors include 1.194 for the MA PD plan, 0.887 for PDPs, and 1.202 for the PACE-only version.
Finally, Medicare will begin negotiating drug prices for a total of ten drugs in 2026, with the negotiated prices impacting costs starting that year. These negotiated prices, known as Maximum Fair Prices (MFPs), will represent net prices and will affect risk scores in the updated Part D model. These changes are part of a broader effort to reduce prescription drug costs and improve affordability for Medicare beneficiaries, including the maximum fair price established for these drugs through medicare drug price negotiation.
Cap on Out-of-Pocket Prescription Drug Costs
In 2026, the out-of-pocket cap for prescription drugs under Part D will increase to $2,100, up from $2,000 in 2025. This increase reflects adjustments based on average drug expenditures from previous years and aims to keep pace with rising drug costs. For many Medicare beneficiaries, this change will provide some relief by capping their maximum out-of-pocket spending on prescription drugs.
Once beneficiaries reach the out-of-pocket spending limit, they will not incur any additional charges for covered prescriptions. This policy ensures that once a beneficiary has spent $2,100 on prescription drugs in a year, they can access their medications without further financial burden. This annual adjustment is designed to ensure that the cap remains relevant and reflective of changes in drug prices over time.
Capping out-of-pocket costs aims to alleviate the financial strain on beneficiaries who require ongoing prescription medications and help them save money. This change is part of a broader effort to make prescription drugs more affordable and accessible for all Medicare enrollees.
Compare Medicare Plans & Rates in Your Area
Insulin Cost Cap

Starting in 2026, Medicare Part D will introduce a new rule capping the cost-sharing for insulin at $35 per month. This change is designed to reduce the financial barriers for patients who rely on insulin, ensuring that they can afford this essential medication without undue hardship.
Under this new policy, beneficiaries will pay a maximum of $35 for a one-month supply of covered insulin, regardless of the insulin product. This cost-sharing amount will not exceed 25% of the maximum fair price or the negotiated price, providing additional protection against high out-of-pocket costs. Furthermore, no deductible will be applied to insulin costs for Medicare beneficiaries, making insulin more affordable from the start of the year.
The insulin cost cap applies to all forms of insulin covered under Medicare, ensuring consistent affordability across different types of covered insulin products. This change is a significant step towards making essential medications more accessible and reducing the financial burden on Medicare beneficiaries.
Zero Cost-Sharing for Adult Vaccines
In 2026, Medicare Part D will implement a zero cost-sharing policy for adult vaccines recommended by the Advisory Committee on Immunization Practices (ACIP). This policy ensures that beneficiaries can access vital vaccines without any out-of-pocket costs, promoting better public health outcomes.
The list of vaccines covered under this policy includes those specifically recommended by ACIP, and it will be subject to annual updates to reflect the latest immunization practices. This means that beneficiaries can stay up-to-date with their vaccinations without worrying about the cost, supporting overall health and wellness.
Moreover, the Medicare Part D deductible does not apply to these vaccines, ensuring that beneficiaries can receive them at no cost starting from the first day of the year. By removing financial barriers to vaccination, this policy aims to increase vaccination rates and protect more people from preventable diseases.
Medicare Prescription Payment Plan Auto-Renewal

Starting in 2026, the Medicare drug plan Prescription Payment Plan will automatically renew enrollees’ participation each year unless they choose to opt out. This change is designed to simplify the process for beneficiaries and ensure continuous coverage without the need for annual re-enrollment.
The opt-out process will be streamlined to make it easier for users to navigate. Participants can still review their plan annually and make changes if needed, but the auto-renewal feature provides peace of mind that their prescription payment plan will remain active unless they decide otherwise.
This change is part of an ongoing effort to improve the user experience for Medicare beneficiaries.
Limits on Special Supplemental Benefits for Chronic Illnesses
In 2026, Medicare Advantage plans will face new limits on special supplemental benefits for chronically ill individuals. These limits are designed to establish clear guidelines for what can be considered health-related support, ensuring that the defined standard benefit provided is genuinely beneficial to beneficiaries’ health.
The finalized rules include a codified list of items that cannot be classified as health-related support. For example, unhealthy food options, alcohol, and tobacco are explicitly excluded from being considered as health-related support. This proposed rule aims to ensure that the benefits offered truly support the health or overall function and well-being of beneficiaries, as outlined in the final rule, creating a reasonable expectation of support.
By streamlining the benefits and establishing clear guardrails, Medicare aims to provide more effective support to those with chronic illnesses. This change reflects a broader effort to enhance the quality and relevance of supplemental benefits provided by Medicare Advantage plans.
Annual Review of Medicare Plans
It’s essential for Medicare beneficiaries to review their plans annually to assess their options, costs, and benefits. Costs, benefits, and providers can change yearly, making regular reviews necessary to ensure that beneficiaries are getting the best possible coverage for their needs.
Each year, beneficiaries have the opportunity to join, switch, or drop their Medicare plans during the annual election period. After this period, enrollees will receive a notice detailing the terms and conditions of their renewed plan, ensuring they are fully informed about any changes. This review process is crucial for adapting to changes in lifestyle, health status, and healthcare needs.
Changes in lifestyle, such as moving to a new location or reaching a certain age, can impact Medicare coverage needs. Additionally, health status changes, including new diagnoses or injuries, may require adjustments in Medicare plans to ensure adequate coverage. By regularly reviewing their plans, beneficiaries can make informed decisions that significantly impact their overall healthcare costs in retirement.
Compare 2026 Plans & Rates
Enter Zip Code
Summary
As we look ahead to 2026, the changes to Medicare are poised to bring significant improvements to the program. From increased payments to Medicare Advantage plans to new caps on out-of-pocket prescription drug costs, these updates aim to enhance the affordability and accessibility of healthcare for Medicare beneficiaries.
Staying informed about these changes is crucial for making the most of your Medicare coverage. By understanding the new policies and how they impact your benefits, you can better navigate the system and ensure that you receive the care you need. Remember, knowledge is power, and staying up-to-date with Medicare changes will help you make the best decisions for your health and financial well-being.
Frequently Asked Questions
What is the maximum monthly cost for insulin for Medicare beneficiaries starting in 2026?
Starting in 2026, the maximum monthly cost for insulin for Medicare beneficiaries will be $35, with no deductible required.
What cost-sharing policy is implemented for adult vaccines under Medicare Part D?
Starting in 2026, adult vaccines recommended by the Advisory Committee on Immunization Practices will have zero cost-sharing under Medicare Part D. This policy ensures that recipients can access necessary vaccinations without any out-of-pocket expenses.
What opportunities do Medicare beneficiaries have each year regarding their plans?
Medicare beneficiaries have the opportunity each year to join, switch, or drop their Medicare Advantage or Part D drug plans, or switch to Original Medicare during the annual election period. This flexibility allows beneficiaries to adjust their coverage according to their changing healthcare needs.
What changes will Medicare Advantage plans face in 2026 regarding supplemental benefits?
In 2026, Medicare Advantage plans will implement restrictions on special supplemental benefits for chronic illnesses, specifying which services will not qualify as health-related support. This change emphasizes the need for beneficiaries to understand their coverage options carefully.
What will the out-of-pocket cap on prescription drugs under Part D be in 2026?
The out-of-pocket cap on prescription drugs under Part D will be $2,100 in 2026. This increase reflects adjustments to help manage costs for beneficiaries.
Speak to the Professionals about Medigap Plans and Original Medicare
If you find understanding the benefits involved with Original Medicare and Medigap Plans challenging, you’re not alone. Whether it’s a Medigap plan, or you want to know more about the Changes to Medicare in 2026, we can help. Call our team at 1-888-891-0229 for a free consultation or complete the contact form on this site, and an expert will call you back at a convenient time.
We have decades of experience advising our clients on the complexities of Medicare and Medigap plans, the benefits, costs and deductibles. We’ll ensure you get the best rate in your state and advice you can trust.