by Russell Noga | Updated March 15th, 2024
Discover the latest updates to Philadelphia American Medicare Supplement plans, specifically the Philadelphia American Medicare Supplement 2025, including new benefits and cost changes. Whether you need enhanced coverage or are budgeting for the coming year, this article delivers the specifics you’re looking for. We pinpoint the adjustments that could impact your choice and help you anticipate how these changes align with your healthcare requirements.
Key Takeaways
- Philadelphia American Medicare Supplement Plans for 2025 fill the gaps in Original Medicare, offering reliable coverage along with extra benefits like vision, dental, and emergency international coverage, with a variety of plans like A, B, C, F, G, N, and high deductible options to meet diverse healthcare needs.
- Costs for Philadelphia American Medigap plans are influenced by location, age, gender, tobacco use, and may offer household discounts, but beneficiaries should also consider factors such as rate increases and non-standardized perks in comparison to other providers.
- During the Medicare Open Enrollment Period (October 15 to December 7), beneficiaries can change their plans, and it is crucial to review coverage annually, taking note of key dates, deadlines, and available financial assistance programs for those with lower income.
Compare 2025 Plans & Rates
Enter Zip Code
Understanding Philadelphia American Medicare Supplement Plans for 2025
As the healthcare needs of individuals continue to diversify, Philadelphia American steps up to the plate with its range of Medicare Supplement Plans for 2025. These plans, also known as Medigap policies, are designed to fill the gaps left by Original Medicare, offering beneficiaries the assurance of comprehensive coverage. With a variety of Medicare supplement policies tailored to cater to different needs, from the cost-conscious individual to the globetrotter seeking international emergency care, understanding the nuances of these offerings is the first step in safeguarding your health and finances.
In the labyrinth of healthcare options, Philadelphia American illuminates the path with its Medigap policies, known for their:
- flexibility and reliable coverage
- lenient underwriting process that opens doors for many with pre-existing conditions
- absence of declinable drug lists, meaning your medication regimen won’t disqualify you from coverage
- reputation for speedy claims processing
- guaranteed renewability of policies
Philadelphia American stands as a beacon of stability in the ever-shifting tides of healthcare.
Plan Offerings
Philadelphia American offers a medley of Medicare Supplement Plans, including the widely favored Plans A, B, C, F, G, and N, each with its own symphony of benefits. The iconic Plan F, for instance, strikes a harmonious balance between cost and convenience, allowing beneficiaries to enjoy healthcare without the worry of out-of-pocket expenses after the premium, as long as services are approved by Medicare. The freedom to select any hospital or doctor that accepts Medicare without the need for referrals is a testament to the flexibility and broad coverage offered.
For those who prefer to hedge their healthcare bets with a high deductible option, the High Deductible Plan F hits the right notes with identical benefits to the standard Plan F, yet with significant cost savings upfront. With a deductible of $2,490 for the year 2025, this plan caters to those willing to pay lower premiums in exchange for a higher initial cost share before the plan’s benefits kick in. Such a diverse ensemble of plans ensures that whether you’re seeking full coverage or strategic cost management, there’s a plan to suit your individual healthcare symphony.
Prescription Drug Coverage
When it comes to prescription drug coverage, Philadelphia American’s Medicare Supplement Plans harmonize with new legislation aimed at lifting the financial burden of medications for Medicare beneficiaries. A noteworthy measure effective from January 2023 is the cap on insulin costs, ensuring that individuals with diabetes can access their insulin for no more than $35 for a one-month supply, a significant stride toward affordable care.
Furthermore, the new prescription drug law has amplified the benefits by eliminating out-of-pocket expenses for vaccines recommended by the Advisory Committee on Immunization Practices for those with a Medicare Part D prescription drug plan.
Looking forward, the absence of co-pays, copayments, or coinsurance post-reaching the catastrophic coverage phase and the cap on annual Part D out-of-pocket expenses at $2,000 by 2025 exemplify the commitment to making prescription drugs more accessible to all Medicare beneficiaries.
Additional Benefits
Philadelphia American’s Medicare Supplement Plans go beyond the basics, offering supplemental coverage that caters to a range of specific needs. Vision, dental, and hearing coverage fill in the gaps of Original Medicare, providing a more holistic approach to health maintenance. For globetrotters, the Foreign Travel Emergency Benefit ensures that unexpected illnesses abroad don’t lead to financial distress, covering 80% of emergency care costs up to plan limits after a deductible.
In addition to these supplemental coverages, Philadelphia American extends its care through ancillary products like Final Expense and Critical Illness policies, as well as partnering with Era Life Insurance Company for additional support. The Final Expense policy, a form of whole life insurance, offers peace of mind with level premiums and benefits that bypass probate for beneficiaries. Critical Illness policies provide a safety net with lump sum payments for specific diagnoses, aiding in covering costs that may not be included in traditional health insurance plans. These additional benefits demonstrate Philadelphia American’s commitment to providing comprehensive support for beneficiaries’ diverse and evolving healthcare needs.
Comparing Philadelphia American with Other Providers
In the grand orchestra of Medicare Supplement providers, Philadelphia American plays a distinctive tune. To make an informed choice, it’s crucial to compare not only the notes but also the harmony of each provider’s offerings. Let’s examine how Philadelphia American’s coverage options, cost structure, and customer service experience measure up against the medley of other providers in the market, ensuring you can make a choice that resonates with your personal healthcare melody.
Whether it’s the depth of coverage or the tempo of premium costs, understanding the differences between providers is instrumental in selecting the right plan. While all Medigap plans are federally standardized, offering identical coverage options for the same plan types, nuances like customer service, rate increases, and additional benefits can significantly influence your choice. Let’s delve deeper into the specifics of how Philadelphia American stands out from the ensemble of providers.
Coverage Options
The coverage options offered by Philadelphia American include:
- Medicare Supplement plans that are federally standardized
- Ability to be used with any doctor or hospital that accepts Medicare, liberating beneficiaries from the constraints of network restrictions
- Consistent claims processing experience through the Medicare ‘crossover’ system
These features make Philadelphia American’s Medigap policies stand out in the marketplace.
However, it’s the extra measures that can make a provider’s coverage sing. Some competitors, like AmeriHealth, may offer additional benefits such as gym memberships or routine vision and hearing exams within their Medicare Advantage plans. While Philadelphia American focuses on core Medigap benefits, the absence of such non-standardized perks in its offerings can be a point of consideration for beneficiaries who value these extras. It’s essential to weigh the melody of coverage options in harmony with your healthcare needs when orchestrating the right choice.
Cost and Premiums
The cost of premiums plays a pivotal role in the medley of factors influencing the choice of a Medicare Supplement plan. Philadelphia American’s premiums, like a concerto, may vary based on a multitude of factors such as:
- location
- age
- gender
- tobacco use
The company’s provision of household or marital discounts, akin to other providers, can be a sweet refrain in lowering the overall cost of their plans.
The cadence of rate increases is another critical measure in the financial symphony of Medicare Supplement plans. State-approved rate increases are a reality for all providers, including Philadelphia American, and may fluctuate based on claims experience and other factors. The company’s history of conservative rate increases and the potential for rate lock features offer a steadier rhythm in premium costs over time, which can be a decisive factor for beneficiaries when comparing the overall cost-effectiveness with other providers.
Customer Service Experience
The customer service experience is the crescendo that can elevate a provider’s standing in the eyes of beneficiaries. Philadelphia American offers:
- Competitive rates
- A reasonable rate history
- Quick policy issuance
- Commitment to excellent customer service
These factors contribute to beneficiary satisfaction and set a strong foundation for a positive service experience.
Comparatively, established providers such as Mutual of Omaha and Aetna have built reputations for stable customer service experiences, which Philadelphia Americans must measure up against. The company’s long history, the satisfaction expressed by clients with the ease of working with their agents, and the clarity of information provided suggest that Philadelphia American’s customer service experience is hitting the right notes. However, it is worth noting that the company is not BBB accredited, which may influence some beneficiaries’ perceptions.
Compare Medicare Plans & Rates in Your Area
Navigating the Medicare Open Enrollment Period
The Medicare Open Enrollment Period is the grand intermission in the annual healthcare opera, a time when beneficiaries can adjust their coverage to better align with their evolving area of healthcare needs and budget considerations. This period provides the flexibility to switch from Original Medicare to Medicare Advantage, change prescription drug plans, or join a new Medicare Advantage Plan, allowing beneficiaries to fine-tune their coverage as they would the strings of a violin.
To ensure that your healthcare coverage performs in perfect harmony with your needs, the Medicare Plan Finder tool on the Medicare.gov website can be an invaluable resource. It allows beneficiaries to compare the costs and benefits of different Medicare Supplement plans available in their area, ensuring that the chosen plan resonates with their unique healthcare composition.
Key Dates and Deadlines
Mark your calendars, for the Medicare Open Enrollment Period takes center stage from October 15 to December 7 annually. The changes made during this period echo into the following year, with coverage adjustments taking effect on January 1, ensuring that the overture of your healthcare coverage is set to the right tempo for the new year.
As the curtain rises on this critical period, it’s essential to conduct a timely review of your coverage, ensuring you don’t miss a beat. The decisions made during this time can significantly influence your healthcare experience, making it crucial to stay attuned to the key dates and deadlines that govern this period.
Making Changes to Your Plan
The Medicare Open Enrollment Period is not the only time to make changes to your score of healthcare coverage. The Medigap Open Enrollment Period, which begins the first month you turn 65 and are enrolled in Medicare Part B, provides an initial opportunity to fine-tune your coverage without the constraints of medical underwriting. Additionally, within the first three months of having Medicare Part A and Part B, if enrolled in a Medicare Advantage Plan during the Initial Enrollment Period, beneficiaries can change to another Medicare Advantage Plan or revert to Original Medicare. Understanding the different Medicare parts can help you make the best decision for your healthcare needs.
Beyond these periods, life’s unforeseen improvisations, such as moving or losing other insurance coverage, may qualify you for a Special Enrollment Period. Starting from January 1, 2024, these occurrences open a two-month window to join or switch plans, offering a fortissimo of flexibility in the face of change.
Evaluating your healthcare needs, especially in anticipation of significant medical events or medical conditions, is pivotal as it can dramatically influence the decisions you make when selecting a Medicare Supplement plan.
Financial Assistance and Support Programs
The melody of Medicare coverage should be harmonious for all, regardless of financial standing. For those facing the crescendo of low income, there is a suite of financial assistance and support programs designed to help cover the costs of Medicare Supplement plans. Medicaid and Medicare Savings Programs serve as a duet of support for eligible beneficiaries, providing a safety net that complements the coverage provided by Medigap policies.
For those struggling with the costs associated with prescription drugs, the Part D Low-Income Subsidy, also known as Extra Help, brings relief with its financial aid, ensuring that essential medications remain accessible and affordable. These programs represent the commitment to a harmonious healthcare system where financial barriers do not impede the ability to receive comprehensive coverage.
Medicaid and Medicare Savings Programs
Medicaid and Medicare Savings Programs are the ensemble of assistance that harmonizes with the needs of beneficiaries requiring financial support. These programs, including the Qualified Medicare Beneficiary (QMB), Specified Low-Income Medicare Beneficiary (SLMB), Qualifying Individual (QI), and Qualified Disabled & Working Individual (QDWI) programs, offer various levels of aid to help with premiums, deductibles, coinsurance, and copayments.
Eligibility for these programs is orchestrated by income and resource limits, which are adjusted annually to accommodate the changing economic landscape. For example, the QMB Program covers a comprehensive range of costs and sets income limits for individuals at $1,275 per month, with resource limits at $9,430 as of 2024. Knowing the nuances of these programs can be the key to unlocking the door to affordable healthcare coverage.
Part D Low-Income Subsidy
For many, the Part D Low-Income Subsidy, affectionately known as Extra Help, plays a pivotal role in the allegro of managing prescription drug costs. This program conducts a symphony of support, harmonizing the financial aspects of Medicare prescription drug coverage for eligible beneficiaries, setting an income limit at up to $1,903 monthly for an individual and offering substantial disregard for certain income and assets.
The crescendo of benefits from this program includes:
- The subsidization of the Part D premium up to benchmark amounts
- The lowering of prescription costs Starting in 2024, the LIS program expands its reach, setting:
- Cost caps for generic and brand-name drugs
- Automatically enrolling beneficiaries in a Part D plan if they don’t choose one, ensuring uninterrupted coverage and access to necessary medications.
Tips for Choosing the Right Medicare Supplement Plan
Choosing the perfect Medicare Supplement plan can be likened to selecting the right instrument for a musical composition—it must resonate with the performer’s style and the piece’s overall mood. With an array of Medicare Supplement plans available, it becomes essential to align them with individual health needs and financial considerations to ensure the best possible coverage. To navigate this selection process with finesse, consider these tips that strike the right chord in selecting the Medicare Supplement plan that orchestrates the best harmony for your healthcare needs.
It’s a prudent practice to review Medicare Supplement plans annually, as changes in health needs and plan benefits may occur over time. This ongoing review ensures that your selected plan continues to provide the coverage you require and adapts to any changes in your health status or financial situation, keeping your healthcare coverage in perfect pitch with your life’s evolving melody.
Assessing Your Healthcare Needs
The prelude to choosing the right Medicare Supplement plan begins with a thorough assessment of your healthcare needs. Reflect on your current health status, medical history, and potential future healthcare requirements. Understanding your family medical history can offer insights into potential health conditions that might surface in the future, affecting your healthcare needs and influencing the coverage you should consider.
Anticipating potential healthcare scenarios, such as the need for hospitalization or specialized services, can help you choose a Medigap plan that covers those expenses. Medigap policies offer the flexibility to change coverage based on your evolving healthcare needs, allowing you to seek more benefits or less costly policies or even switch insurers to better match your healthcare composition.
Comparing Costs and Benefits
When the score of Medicare Supplement plans is before you, it’s critical to conduct a detailed comparison of costs and benefits. Look beyond the initial premium and consider the potential rate increases, deductibles, copayments, and coinsurance that can affect your financial harmony. Calculating the annual costs, including premiums and any other out-of-pocket expenses, will provide you with a total expenditure to evaluate the true cost of a plan.
Assessing the value of the benefits relative to the cost is akin to weighing the notes in a musical piece. How likely you are to use various covered services should influence your decision, as well as coverage for extra services like at-home recovery, preventive care, or vision and dental services if they align with your healthcare priorities and offer benefits.
Consult with Professionals
Sometimes, the most harmonious decisions are made with a conductor at the helm. Consulting with professionals, such as Medicare-licensed insurance agents or brokers, can provide personalized guidance in choosing the best Medicare Supplement plan for you. Our experts can be particularly beneficial during medical underwriting for Medicare Supplement Insurance policies outside the open enrollment period.
Summary
In the grand composition of healthcare coverage, Philadelphia American Medicare Supplement Plans for 2025 offer a harmonious blend of coverage, flexibility, and additional benefits. As we’ve explored the nuances of these plans, compared them with other providers, navigated the open enrollment period, and uncovered financial assistance programs, it’s clear that the right Medicare Supplement plan is a pivotal movement in the symphony of your healthcare journey.
Armed with the knowledge from this guide, you are now ready to conduct your healthcare coverage with confidence. Whether it’s assessing your healthcare needs, comparing costs and benefits, or seeking professional consultation, each step is an essential note in the melody of making an informed decision that ensures your healthcare coverage is in perfect concert with your life.
Compare 2025 Plans & Rates
Enter Zip Code
Frequently Asked Questions
Is Philadelphia American a Medicare supplement?
Yes, Philadelphia American offers Medicare Supplement insurance nationwide with a focus on quick policy issuance and exceptional customer service.
What kind of insurance is Philadelphia American?
Philadelphia American is a subsidiary of New Era Life Insurance Company, which specializes in health insurance and offers Medicare Supplement insurance across the United States, including annuities, life, health, and disability insurance products and services.
Does Philadelphia American pay for Medicare deductible?
Yes, Philadelphia American Medigap insurance covers Medicare deductibles, copayments, and coinsurance to help reduce out-of-pocket costs.
Who owns Philadelphia American Life?
Philadelphia American Life is owned by New Era Life Insurance Company, a larger insurance firm based in Houston, Texas.
Can I choose any doctor or hospital with Philadelphia American Medicare Supplement Plans?
Yes, you can choose any doctor or hospital that accepts Medicare without network restrictions, providing you with freedom and flexibility in your healthcare choices.
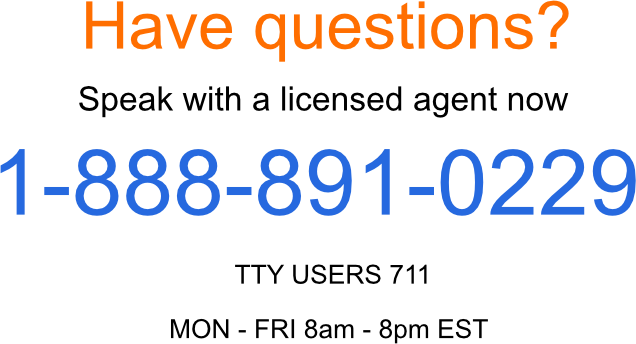
Speak to the Professionals about Medigap Plans and Original Medicare
If you find understanding the benefits involved with Original Medicare and Medigap Plans challenging, you’re not alone. Whether it’s a Medigap plan, or you want to know more about Philadelphia American Medicare Supplement in 2025, we can help. Call our team at 1-888-891-0229 for a free consultation or complete the contact form on this site, and an expert will call you back at a convenient time.
We have decades of experience advising our clients on the complexities of Medicare and Medigap plans, the benefits, cost and deductibles. We’ll ensure you get the best rate in your state and advice you can trust.