
by Russell Noga | Updated January 22th, 2024
If you’ve ever experienced the unexpected rush of a leaky bladder, you’re not alone. Millions of American adults face the challenges of urinary incontinence, a condition often associated with age, illness, or disability.
Finding the right incontinence supplies can be a daunting task, especially when financial constraints come into play.
But here’s the good news: there are options available to help offset the costs, and understanding your Medicare and Medicaid benefits is a good place to start. So let’s dive in and untangle the knots of incontinence supplies covered by Medicare coverage!
Key Takeaways
- Original Medicare (Parts A and B) doesn’t cover incontinence supplies, as these are not classified as medically necessary; whereas Medicare Advantage (Part C) plans may offer coverage, depending on the specific plan.
- Medicaid, a state-run insurance program for low-income individuals, often provides coverage for incontinence supplies, though benefits can vary significantly from state to state.
- Private insurance policies vary widely and may not cover incontinence supplies, necessitating the evaluation of various plans or considering other cost-saving measures such as FSAs, coupons, or non-profit organizations.
Understanding Medicare and Incontinence Supplies

Medicare, a health insurance program offered by the U.S. federal government, is a lifeline for many Americans. It provides coverage for a range of medical supplies, but when it comes to incontinence supplies, the scenario changes.
If you’re relying on Original Medicare (Parts A and B), you may be disappointed to learn that it doesn’t cover incontinence supplies. You might wonder why Medicare does not cover incontinence supplies.
The reason is rooted in Medicare’s eligibility rules that classify these supplies as non-essential, hence they are not covered.
However, don’t lose hope yet. Medicare Advantage plans, also known as Part C, may come to your rescue.
Provided by private insurance companies, these plans often offer broader coverage options, which might include incontinence supplies, depending on the specific plan and service area.
Original Medicare and Incontinence Supplies
Original Medicare primarily covers hospital and medical insurance (Parts A and B, respectively). It provides coverage for a wide range of healthcare services and supplies, but unfortunately, incontinence supplies miss the list.
The rationale behind this exclusion is that Medicare does not consider incontinence supplies as medically necessary, hence the lack of coverage.
This implies that if your only insurance is Original Medicare, you will have to shoulder the cost of incontinence supplies yourself. Given the high prices of these supplies, this fact can be startling for many.
Hence, planning for this coverage gap becomes imperative.
Medicare Advantage Plans and Incontinence Supplies
Unlike Original Medicare, Medicare Advantage plans are potentially more flexible when it comes to covering incontinence supplies. These plans are provided by private insurance companies under Part C of Medicare.
However, it’s important to note that not all Medicare Advantage plans are the same. Coverage varies widely depending on the specific plan and the service area in which it is offered.
So, if you’re contemplating a Medicare Advantage plan, thoroughly reviewing your plan’s benefits or directly reaching out to the plan for more details becomes essential. This will give you a clear understanding of whether your plan covers incontinence products and what you might expect to pay for them.
Compare 2024 Plans & Rates
Enter Zip Code
Medicaid and Incontinence Supplies

Now, if Medicare isn’t an option for you, don’t worry. Medicaid might be your saving grace. Medicaid is a state-run insurance option.
It is available to low-income adults, children, seniors, and people living with disabilities. Unlike Medicare, Medicaid can provide coverage for incontinence supplies.
Nonetheless, keep in mind that both eligibility and benefits can differ from one state to another.
One of the key differences between Medicaid and Medicare is the flexibility Medicaid offers regarding incontinence supplies. While Medicare has strict regulations concerning these supplies, Medicaid is often more lenient, offering coverage based on individual state guidelines.
However, keep in mind that there could be brand limitations for incontinence supplies covered by Medicaid.
State Differences in Medicaid Coverage
A crucial factor to consider when relying on Medicaid for incontinence supplies is the state you reside in. Medicaid coverage varies by state, with each one having its set of rules and regulations.
The coverage can range from comprehensive to limited benefits, and some states may have stringent requirements. For instance, some states might require proof of medical necessity or limit the number of incontinence products you can receive in a month.
Typically, state Medicaid programs cover medically necessary incontinence supplies such as boosters and adult diapers. However, the specifics of Medicaid cover incontinence supplies may vary depending on the state’s Medicaid program.
Hence, reaching out to your state’s Medicaid program to ascertain the precise coverage details becomes necessary. It’s also worth checking if Medicare cover adult diapers in your specific situation.
Applying for Medicaid Coverage
Applying for Medicaid coverage requires meeting certain eligibility requirements. These requirements vary from state to state and may include income limits and residency requirements.
To apply for Medicaid coverage, you’ll need to provide documents that demonstrate your eligibility. These documents may include proof of income, bank records, property documents, retirement account statements, insurance information, car registration, and burial documents.
The enrollment process for Medicaid might seem daunting, but help is available. You can reach out to your state’s Medicaid office for guidance and assistance.
It’s also a good idea to contact a supplier who is familiar with Medicaid coverage for incontinence supplies, as they can help you navigate the process and understand your benefits.
Private Insurance Options for Incontinence Supplies

If Medicare and Medicaid aren’t viable options for you, private insurance could be the answer. Private insurance plans encompass any health insurance coverage that does not depend on state or federal government support.
These plans are typically offered by employers or purchased directly by individuals. Private insurance policies, like Medicare Advantage plans, usually include coverage for various medical services and supplies, such as covers durable medical equipment.
This can encompass prescription drugs, durable or disposable medical equipment (DME), and hospital stays. But when it comes to incontinence supplies, the Medicare coverage varies by company.
It’s important to remember that private insurance policies differ greatly in terms of coverage, costs, and benefits. Thus, if you’re weighing private insurance for incontinence supplies, it becomes vital to contrast different plans and select one that aligns best with your needs and budget.
Types of Private Insurance Plans
When exploring private insurance options, you’ll find a variety of plans. However, remember that Medicare and most private insurance plans do not provide coverage for incontinence supplies.
The coverage for these supplies is influenced by differences in policy between Medicare and Medicaid, federal and state regulations, and individual contracts with healthcare providers.
One possible solution is a flexible spending account (FSA). An FSA is a special account you put money into that you use to pay for certain out-of-pocket healthcare costs, including incontinence products.
This can be a great way to set aside money tax-free for incontinence supplies if your insurance doesn’t cover them.
Comparing Private Insurance Plans
Choosing a private insurance plan is a significant decision and should be done thoughtfully. When scrutinizing private insurance plans, it is critical to evaluate factors like:
- Network coverage
- Prescription drug coverage
- Additional benefits
- Supplemental insurance options
- Preferred doctors and hospitals in the plan’s network
- Cost
- Convenience
- Coverage
- Customer service
As mentioned earlier, most private insurance plans do not provide coverage for incontinence supplies.
The claim process for incontinence supplies can also vary among private insurance companies. It’s crucial to collaborate with your healthcare provider to ensure the appropriate documentation is submitted in accordance with the insurer’s policies.
Cost-Saving Strategies for Incontinence Supplies

While we’ve talked about insurance coverage options for incontinence supplies, let’s not overlook the importance of cost-saving strategies. After all, any opportunity to save money is worth considering, right?
Cost-saving strategies can range from shopping online and using coupons to leveraging local resources and non-profit organizations. These strategies can help offset the costs of incontinence supplies, especially if you’re paying out of pocket.
Remember, every little bit helps. By combining a few of these strategies, you might find that the financial burden of managing incontinence becomes a little easier to bear.
Online Shopping and Couponing
One of the simplest ways to save on incontinence supplies is to shop online. Online shopping offers several advantages, including:
- the ability to compare prices
- read product reviews
- purchase items in bulk at discounted prices
- it’s discreet and convenient – you can shop from the comfort of your home and have your supplies delivered right to your doorstep.
Coupons can also provide significant savings. Websites like lozo.com, needymeds.org, and wellnessbriefs.com often feature coupons for incontinence supplies.
By combining online promotions and sales with coupons, you could significantly reduce the cost of your incontinence supplies.
Local Resources and Non-Profit Organizations
Let’s not forget about local resources and non-profit organizations. Many communities have organizations that offer free or low-cost incontinence supplies, as well as other incontinence supplies, to those in need.
These resources can be a lifeline for individuals struggling to afford the cost of incontinence supplies.
Non-profit organizations, such as adult diaper banks, distribute low-cost incontinence supplies, including cover adult diapers, through local nonprofit agencies and religious organizations. They also provide information and support to those affected by incontinence, making them a valuable resource for those managing this condition.
Incontinence Treatment Options Covered by Medicare

While the battle to cover incontinence products and incontinence supplies continues, it’s comforting to know that Medicare does provide coverage for various incontinence treatments.
These treatments can help manage the symptoms of incontinence, improve your quality of life, and potentially reduce your reliance on Medicare cover incontinence supplies.
So, what type of incontinence treatments does Medicare cover? Let’s delve into two common treatments: bladder control training and medications.
Bladder Control Training
Bladder control training is a non-invasive technique used to treat urinary incontinence. It involves modifying urination patterns and can be beneficial for conditions like stress incontinence, overactive bladder, or a weak bladder.
The training generally includes scheduled urination to progressively enhance bladder capacity and improve bladder control. In addition to this training, some individuals may also use bladder control pads for added protection and confidence.
Bladder control training can be a game-changer for many individuals, helping them regain control over their bladder and improve their quality of life. It’s important to remember that while this treatment can be effective, it’s not a quick fix and requires commitment and consistency.
Medications for Incontinence
In addition to bladder control training, Medicare provides coverage for medications used to treat incontinence. Medications can help manage the symptoms of incontinence by calming an overactive bladder or improving bladder function.
Coverage for these medications is provided under Part D of Medicare, also known as the prescription drug coverage. If you’re considering this option, it’s important to understand the enrollment process, which involves enrolling on the Medicare Plan Finder or on the plan’s website, completing a paper enrollment form, or even calling the plan directly.
Navigating the Medicare Enrollment Process
Enrolling in Medicare can seem like a daunting task, especially when you’re already dealing with incontinence. However, understanding the process can make it more manageable.
The process begins with determining your eligibility for Medicare. To qualify, you generally need to be 65 or older, although there are exceptions for certain disabilities and conditions.
Once you’ve determined your eligibility, it’s time to dive into the enrollment process. This involves enrolling in Original Medicare (Part A and Part B), and creating your MyMedicare.gov account.
Choosing a Medicare Plan
Choosing a Medicare plan is one of the most critical steps in the enrollment process. Medicare offers several plans, including:
- Original Medicare (Part A and Part B)
- Medicare Advantage (Part C)
- Medicare Prescription Drug Coverage (Part D)
- Medicare Supplement Insurance (Medigap) plans
Each of these plans offers various coverage options and costs, so selecting the one that aligns best with your needs is essential.
Cost is a major factor to consider when selecting a Medicare plan. Not only should you consider the monthly premium, but also the out-of-pocket expenses like deductibles, copayments, and coinsurance.
Also, keep in mind that the plan with the lowest premium may not necessarily be the most cost-effective option, as it may have higher out-of-pocket costs.
Enrolling in Medicare
Once you’ve chosen a Medicare plan, the next step is to enroll. You can do this online, by mail, or in person at your local Social Security office.
You’ll need to provide some documents to prove your eligibility, including a birth certificate, proof of U.S. citizenship or legal residency, and a Social Security card.
The enrollment process typically takes a few weeks, and after your application is approved, you’ll receive your Medicare card in the mail. Keep in mind that there are certain important dates to remember during the enrollment process, including the initial enrollment period, which is the three months before and after your 65th birthday.
Summary
Whether you’re navigating the complexities of Medicare and Medicaid or exploring private insurance options, understanding the coverage options for incontinence supplies is crucial.
Remember, while it can be challenging, there are resources available to help.
From local resources and non-profit organizations to cost-saving strategies and treatment options, you have a wealth of options at your disposal.
Take the time to research your options, connect with healthcare providers, and choose the plan that best meets your needs.
After all, managing incontinence shouldn’t come at the expense of your financial well-being.
Compare 2024 Plans & Rates
Enter Zip Code
Frequently Asked Questions
Is incontinence supplies covered by Medicare?
No, Medicare does not cover incontinence supplies or adult diapers. You may want to check with your state’s Medicaid program for possible coverage.
Can the elderly get free incontinence pads?
Yes, the elderly can often get free incontinence pads through options like Medicaid, diaper banks, and insurance companies, although the supply provided may be limited. It’s recommended to explore these options to see what best fits your needs.
What diagnosis qualifies for incontinence supplies?
To qualify for incontinence supplies, one must have a diagnosis of an underlying medical condition that involves loss of bladder or bowel control.
Can Medicaid cover incontinence supplies?
Yes, Medicaid can provide coverage for incontinence supplies, but eligibility and benefits vary by state.
What are some cost-saving strategies for incontinence supplies?
Consider online shopping, using coupons, and seeking assistance from local resources and non-profit organizations to save on incontinence supplies. These strategies can help you cut down on costs effectively.
Find the Right Medicare Plan for You
Finding the right Medicare Plan in 2024 doesn’t have to be confusing. Whether it’s a Medigap plan or you want to learn more about Medicare coverage, we can help.
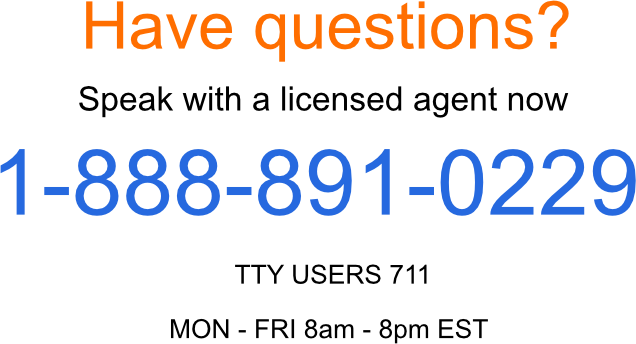
Call us today at 1-888-891-0229 and one of our knowledgeable, licensed insurance agents will be happy to assist you!
Russell Noga is the CEO and Medicare editor of Medisupps.com. His 15 years of experience in the Medicare insurance market includes being a licensed Medicare insurance broker in all 50 states. He is frequently featured as a featured as a keynote Medicare event speaker, has authored hundreds of Medicare content pages, and hosts the very popular Medisupps.com Medicare Youtube channel. His expertise includes Medicare, Medigap insurance, Medicare Advantage plans, and Medicare Part D.


