
by Russell Noga | Updated December 5th, 2023
How Often Does Medicare Pay for Colonoscopy Screening?
Colonoscopy screenings play a crucial role in the early detection and prevention of colorectal cancer, the third most common cancer in the United States. Understanding “how often does Medicare pay for colonoscopy” screenings can help you make informed decisions about your healthcare and reduce out-of-pocket costs.
In this blog post, we will delve into the details of Medicare’s coverage for colonoscopy screenings, the differences between screening and diagnostic colonoscopies, and the various supplemental plans that can further assist with the costs of these essential procedures.
Key Takeaways
- Medicare Part B provides coverage for colonoscopy screenings every 24 months to high-risk patients and every 120 months to average-risk patients.
- Screening colonoscopies are covered by Medicare Advantage HMO plans at 100% of the Medicare amount, whereas diagnostic colonoscopies may involve additional costs such as a 15% fee for the patient.
- Medigap plans can help cover remaining costs after Medicare pays its portion, making it more accessible and affordable with minimal out of pocket expenses.
Medicare Coverage Frequency for Colonoscopy Screenings
 Medicare provides coverage for colonoscopy screenings, taking into account the patient’s risk level for colorectal cancer.
Medicare provides coverage for colonoscopy screenings, taking into account the patient’s risk level for colorectal cancer.
The frequency of coverage depends on whether the patient is considered high-risk or average-risk for colorectal cancer.
Being aware of the coverage frequency aids in staying informed about healthcare options and facilitates timely screenings.
High-Risk Patients
High-risk patients are those with specific risk factors, such as a personal or family history of colorectal cancer, polyps, or inflammatory bowel disease.
For these patients, Medicare covers colonoscopy screenings every 24 months, or every two years, regardless of age. This frequent screening is vital for individuals at higher risk, enabling early detection and prevention of colorectal cancer.
Take note that Medicare Part B provides coverage for colonoscopy screenings every 24 months for high-risk individuals, including those with a family history of colon cancer.
Medicare aims to promote preventive healthcare and protect its beneficiaries by providing more frequent screenings to high-risk patients.
View Rates for 2024
Enter Zip Code
Average-Risk Patients
Average-risk patients are those without specific risk factors for colorectal cancer. They do not have a personal history of colorectal or family history of colorectal cancer or polyps and are not diagnosed with inflammatory bowel disease.
For average-risk patients, Medicare covers colonoscopies every 120 months or 48 months after a sigmoidoscopy.
A sigmoidoscopy is a less invasive screening test that examines the rectum and lower part of the colon for abnormalities and signs of colorectal cancer.
Medicare promotes regular screenings for early detection and prevention of colorectal cancer in average-risk patients by covering colonoscopies every 120 months.
Understanding the Difference Between Screening and Diagnostic Colonoscopies
Recognizing the difference between screening and diagnostic colonoscopies is important as Medicare provides distinct coverage for each type.
While screening colonoscopies aims to prevent colorectal cancer by detecting the disease in its early stages, diagnostic colonoscopies help identify and address existing issues. Understanding these differences can enhance your knowledge of coverage options and potential expenses.
Medicare Advantage HMO plans typically cover colonoscopy screenings as a preventive service with no cost to the patient.
However, diagnostic colonoscopies may involve additional costs, such as a 15% fee for the patient, as Medicare covers 80% of the costs. If a polyp or other abnormality is discovered during a screening colonoscopy, the procedure becomes diagnostic, and patients must pay the 15% Part B coinsurance, as Medicare covers 80% of the cost.
Screening Colonoscopies
Medicare’s coverage for screening colonoscopies is comprehensive. Here are the details:
- Original Medicare covers these procedures at 100% of the Medicare-approved amount, with no minimum age restriction.
- For average-risk patients, Medicare covers colonoscopies every 10 years.
- High-risk patients are eligible for coverage every 24 months.
However, Medicare may not cover 100% of a screening colonoscopy if it is not performed at the recommended intervals or if the individual is not considered at high risk for colorectal cancer.
If a covered colonoscopy is attempted but cannot be completed due to extenuating circumstances, Medicare will still pay for the interrupted colonoscopy.
Diagnostic Colonoscopies
For diagnostic colonoscopies, Medicare covers 80% of the costs, while the patient is responsible for the remaining 20% of coinsurance.
Diagnostic colonoscopies are performed when a patient presents with signs or symptoms of a gastrointestinal disorder, such as rectal bleeding, abdominal pain, or diarrhea.
It’s essential to be aware that diagnostic colonoscopies may involve out-of-pocket costs, such as the Part B deductible and a 20% coinsurance after the deductible has been met.
By understanding the coverage differences between screening and diagnostic colonoscopies, you can better prepare for any potential costs associated with these essential procedures.
Additional Colorectal Cancer Screening Tests Covered by Medicare
 In addition to colonoscopies, Medicare covers three alternative colorectal cancer screening tests for asymptomatic, average-risk patients:
In addition to colonoscopies, Medicare covers three alternative colorectal cancer screening tests for asymptomatic, average-risk patients:
- Fecal Occult Blood Test (FOBT),
- Flexible Sigmoidoscopy,
- and Barium Enema.
Coverage varies by test type and patient age, so it’s crucial to understand the options available to ensure early detection and prevention of colorectal cancer.
Costs and Coverage for Colonoscopy-Related Services
Besides colonoscopy screenings, Medicare covers certain colonoscopy-related services, such as:
- anesthesia,
- and colonoscopy prep kits.
However, coverage and costs may vary, depending on the service type and the specific Medicare plan you have.
Understanding the coverage for these related services can help you minimize out-of-pocket expenses and ensure a smooth colonoscopy experience.
Anesthesia Coverage
Medicare Part B covers anesthesia during colonoscopy screenings, provided the doctor or other provider accepts Medicare. Anesthesia coverage can significantly reduce the costs associated with colonoscopy screenings, making the procedure more accessible to patients.
However, additional copayments may be required, and some plans may need prior authorization for anesthesia coverage. Reviewing your specific Medicare plan and consulting with your healthcare provider about additional requirements is crucial to ensure appropriate anesthesia coverage during colonoscopies.
Colonoscopy Prep Kit Coverage
Medicare covers prescription colonoscopy prep kits, which are essential for properly preparing for a colonoscopy screening. However, Medicare does not cover over-the-counter medications used for colonoscopy preparation.
Checking with your specific Medicare plan is necessary to comprehend the coverage for colonoscopy prep kits, any potential additional costs or copayments, and how Medicare pay factors into the process.
Virtual Colonoscopy Coverage
Currently, Medicare does not cover virtual colonoscopies, a non-invasive procedure that uses a CT scan to generate images of the colon and detect polyps or other irregularities. However, Medicare Part B does cover other types of colorectal cancer screenings, such as screening colonoscopies and Fecal Occult Blood Tests (FOBTs).
Awareness of the coverage limitations for virtual colonoscopies can assist in making informed decisions about colon cancer screening and other colorectal cancer screening options.
Medicare Advantage Plans and Colonoscopy Coverage
Medicare Advantage plans, also known as Part C, offer an alternative way to receive Original Medicare benefits, often with additional coverage for diagnostic colonoscopies.
 These plans are required to cover at least the same benefits as Original Medicare, including colonoscopy screenings. However, coverage for colonoscopy-related services and diagnostic colonoscopies may vary among different Medicare Advantage plans.
These plans are required to cover at least the same benefits as Original Medicare, including colonoscopy screenings. However, coverage for colonoscopy-related services and diagnostic colonoscopies may vary among different Medicare Advantage plans.
Reviewing the specifics of your Medicare Advantage plan is crucial for understanding the coverage for colonoscopy screenings and related services, including whether Medicare cover colonoscopy procedures. By doing so, you can ensure that you receive the necessary preventive care to maintain your health and minimize out-of-pocket expenses.
HMO Plans
Medicare Advantage HMO plans typically offer similar colonoscopy coverage as Original Medicare, with no cost to the patient for screening colonoscopies. However, HMO plans may require a referral from a doctor and preauthorization for colonoscopy screenings.
Understanding the coverage requirements for colonoscopy screenings under HMO plans can facilitate timely access to this preventive service and help minimize potential out-of-pocket costs.
Other Plan Types
Other Medicare Advantage plan types that may cover colonoscopy screenings and related services include:
- Preferred Provider Organizations (PPOs)
- Private Fee-for-Service (PFFS) plans
- Special Needs Plans (SNPs)
- Medical Savings Accounts (MSAs)
Coverage for colonoscopies under these plans is comparable to that of Original Medicare cover, but specific details may vary between different plan types.
Reviewing the coverage details of your specific Medicare Advantage plan is necessary to understand the costs and coverage for colonoscopy screenings and related services.
By doing so, you can ensure adequate preventive care and minimize out-of-pocket expenses.
Medigap Plans and Colonoscopy Costs
Medigap plans, also known as Medicare Supplement plans, help cover the remaining costs of colonoscopy screenings after Medicare pays its portion.

These plans can significantly reduce out-of-pocket expenses for beneficiaries, making colonoscopy screenings more accessible and affordable.
For example, if a screening colonoscopy is deemed diagnostic due to the discovery of a polyp, the patient would be responsible for a 15% Part B coinsurance. In this case, a Medigap plan could help cover the remaining costs, ensuring minimal out-of-pocket expenses for the beneficiary.
Summary
Understanding the intricacies of Medicare’s coverage for colonoscopy screenings and related services is essential for maintaining your health and minimizing out-of-pocket costs.
By familiarizing yourself with the various plan options, coverage frequencies, and alternative colorectal cancer screening tests, you can effectively navigate your healthcare journey and ensure access to crucial preventive care.
Stay proactive about your colorectal health and make informed decisions about your healthcare coverage.
Get Quotes Right Now
Enter Zip Code
Frequently Asked Questions
At what age does Medicare stop paying for colonoscopies?
Medicare pays for colonoscopies regardless of age, but the frequency and coverage limits vary depending on risk factors. Most medical organizations in the United States agree that the benefits of screening decline after age 75 and there is little evidence to support continuing screening after age 85.
Does Medicare cover 100% of colonoscopies?
Medicare covers screening colonoscopies once every 24 months for high-risk patients, and once every 120 months or 48 months after a previous flexible sigmoidoscopy for non-high risk patients. Medicare pays 80% of costs associated with diagnostic colonoscopies, while Part B pays 100% of preventive service colonoscopies without copays or coinsurance.
Does Medicare cover colonoscopy in 2023?
Yes, Medicare will cover colonoscopies in 2023 if you are at high risk for colorectal cancer and every 10 years if you are not at high risk. There is no deductible or copayment if your doctor or other health care provider accepts assignment.
How often do you need a colonoscopy after age 70?
After age 70, a colonoscopy is usually recommended every 10 years. You may need one every 5 years after age 60 if your risk of cancer increases. After age 75 (or 80 in some cases), you may no longer need to get the procedure.
How often does Medicare cover colonoscopy screenings for high-risk patients?
Medicare provides colonoscopy screenings for high-risk patients every two years.
Find the Right Medicare Plan for You
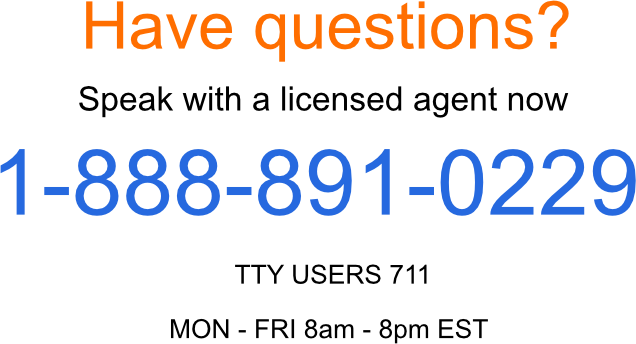
Finding the right Medicare Plan 2024 doesn’t have to be confusing. Whether it’s a Medigap plan, or you want to know how often Medicare pays for colonoscopy screening, we can help.
Call us today at 1-888-891-0229 and one of our knowledgeable, licensed insurance agents will be happy to assist you!
Russell Noga is the CEO and Medicare editor of Medisupps.com. His 15 years of experience in the Medicare insurance market includes being a licensed Medicare insurance broker in all 50 states. He is frequently featured as a featured as a keynote Medicare event speaker, has authored hundreds of Medicare content pages, and hosts the very popular Medisupps.com Medicare Youtube channel. His expertise includes Medicare, Medigap insurance, Medicare Advantage plans, and Medicare Part D.


